A 42 year-old man presents with acute onset fever and chills, with headache, intermittent abdominal pain, and very severe pain in his wrists, ankles, and low back for the past two days. He has no significant past medical history; he lives in Florida and works as an electrician. He has had no recent travel, no recent sexual contacts, and takes no medications. Aside from an occasional mosquito bite, he recalls no significant insect or other animal exposure, recent ill contacts, and has had no known tick bites.
Exam – temperature: 39.0 C, mild tachycardia, ill-appearing, but otherwise without focal findings, including no rashes, joint effusions, and no neurologic findings
Labs – normal CBC and basic chemistry panel, except for mild lymphocytopenia
Discussion
Acute febrile illness challenges clinicians with a very broad differential diagnosis – infectious diseases, collagen vascular diseases, endocrine disorders, to name just a few categories. When fever is associated with hemodynamic stability and generally normal physical findings and initial labs, it is typically attributed to a “viral syndrome” and managed with supportive care and outpatient monitoring. This patient, however, resides in a subtropical region and is showing symptoms and findings which would place a specific emerging vector-borne threat at the top of the differential diagnosis.

Chikungunya
Chikungunya virus is an arthropod-borne single-stranded RNA virus (arbovirus), spread via Aedes mosquitoes, mainly Aedes aegypti and Aedes albopictus.
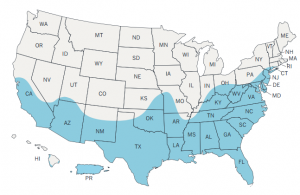
Chikungunya attack rates are very high, with WHO reports as high as 45% in some areas. Endemic to Africa, it spread to the Americas, mainly to the Caribbean, during the 1980s. It is typically spread by travelers, with thousands of documented cases imported to the United States from the Caribbean in 2013 and 2014. There have now been several cases of locally-acquired chikungunya infections (autochthonous) reported in the past few years throughout Florida and most other southern states. Given that the distribution of Aedes mosquitoes includes all of the southern United States, this trend is likely to increase, reinforcing the need to institute excellent vector control programs.
The incubation period for chikungunya infection is two to ten days (most commonly three days) and presents with sudden-onset severe fever, headache, and joint pains. A pruritic maculopapular rash has been observed with variable frequency in several different studies. Fever and other symptoms defervesce over seven to ten days, however, the arthralgias may persist for weeks to months, and in some cases, years.
If the patient presents early in the course of chikungunya infection, as in this case, diagnosis may require viral PCR testing as the IgM antibody response becomes detectable several days to one week after the onset of symptoms. If PCR is unavailable, the patient can be monitored closely to follow the antibody response, first with IgM, and then IgG antibodies.
Treatment of chikungunya is supportive, as there is no specific antiviral medication available. Given that chikungunya and dengue viruses both have the same vector and overlapping clinical features, dengue virus infection needs to be ruled out, especially since dengue fever has a significantly higher case-fatality rate. Until dengue is ruled out, aspirin and non-steroidal anti-inflammatory medications should be avoided, so as not to increase the risk of hemorrhage.
Vector control remains of paramount importance in the prevention not only of chikungunya virus, but of all other known viruses carried by Aedes mosquitoes, including dengue fever, yellow fever, zika, West Nile fever, eastern equine encephalitis, western equine encephalitis, Mayaro fever, Venezuelan equine encephalitis, Japanese encephalitis, and others!
References
CDC (2018), Chikungunya virus, Retrieved from https://www.cdc.gov/chikungunya (Accessed 02 August 2019).
Jameson, J.L., Fauci, A.S., et al, (Eds.)(2018). Harrison’s principles of internal medicine. 20th edition. New York: McGraw-Hill Education.
Thwaites, G.E., Day, N. Approach to fever in the returning traveler. N Engl J Med 2017; 376: 548-560. doi: 10.1056/NEJMra1508435
Weaver, S.C., Lecuit, M. Chikungunya virus and the global spread of a mosquito-borne disease. N Engl J Med 2015; 372:1231-1239. doi: 10.1056/NEJMra1406035