A 28-year-old
man comes to primary care after perusing a health website, which recommended that
he get a screening evaluation for hemochromatosis. It discussed the risk
associated with being of European heritage (which he is), and after reading
more about it, he became anxious and wants to know if he should be checked. He
does not have any of the symptoms listed on the website and does not recall family
members ever discussing it. He has no significant past medical history and
takes no medications.
Exam – normal
Labs – normal CBC, Chem I
Discussion
To screen or
not to screen…
Primary or
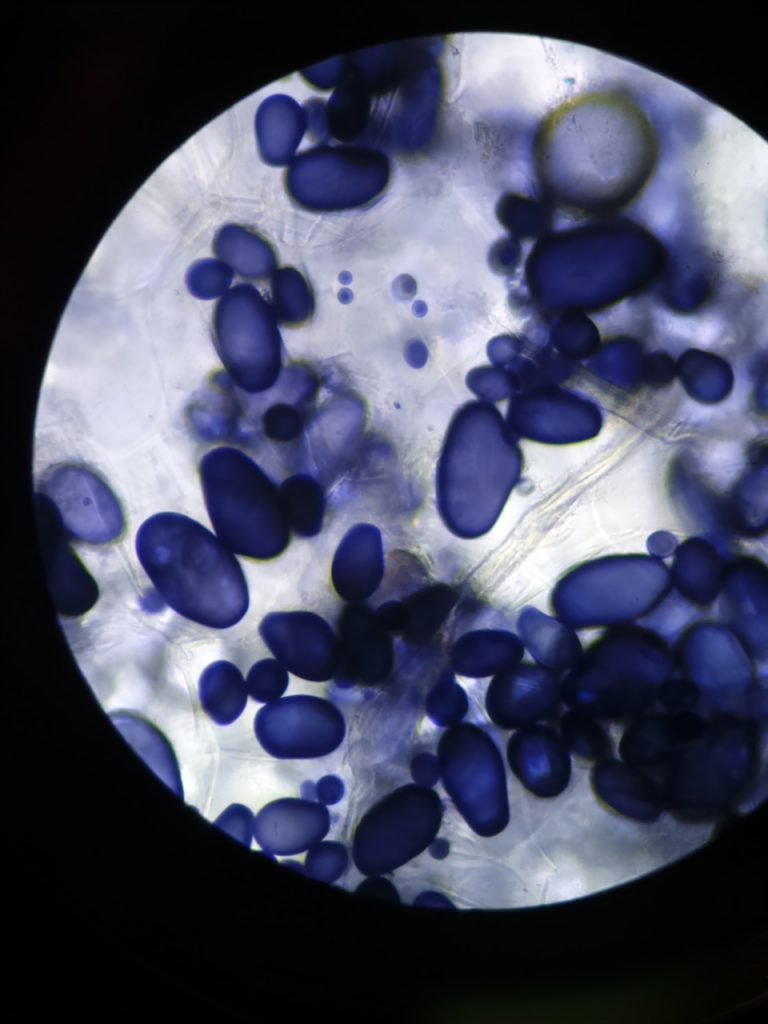
hereditary hemochromatosis is a disorder of iron overload resulting from
genetic mutations that lead to increased iron absorption from the small
intestine. Most cases (about 86%) arise from a mutation in the HFE gene (H for hereditary
hemochromatosis, FE for iron) on chromosome 6. The product of this gene is a
regulator of hepcidin, which in turn, regulates iron metabolism.
The most
common HFE mutation is a nucleotide substitution, guanine to adenine, which causes the amino acid cysteine to be substituted
by tyrosine at position 282 (C282Y). Homozygosity for the mutation is required
to develop iron overload because the normal allele present in heterozygotes makes
sufficient protein to overcome the deficiency from the mutant allele (autosomal
recessive pattern).
A less common HFE mutation causes an
amino acid change from histidine to aspartic acid at position 63 (H63D). Homozygosity
is not associated with clinical disease, but compound heterozygosity (one copy each
of C282Y and H63D) is associated with iron overload.
A third HFE mutation, of less clinical
relevance, involves a serine-to-cysteine amino acid substitution at position 65
(S65C). Also rare are many non-HFE mutations, including hemojuvelin (HJV), hepcidin
antimicrobial peptide gene (HAMP), transferrin receptor 2 (TfR2), and
ferroportin (SLC40A1 – solute carrier family 40 member 1).
Approximately 10% of those with
northern European ancestry are heterozygotes (carriers) for hemochromatosis,
and approximately 0.4 to 0.5% are homozygotes.
The HFE
mutations decrease the function of hepcidin, causing increased duodenal iron uptake,
up to a few milligrams per day above normal. Although a small amount, it is enough
to overwhelm normal daily iron losses of 1-1.5 milligrams. No physiologic
system exists to increase iron excretion in the case of excess. The increased absorption
adds between ten to forty grams of iron over the course of a few decades
(normal total body iron is three to four grams). After overwhelming the storage
capacity of ferritin, free iron accumulates in the liver, pancreas, heart, and
other organs, causing widespread damage.
Women are relatively
protected from iron overload due to losses associated with menstruation and
pregnancy. For example, in an average full-term pregnancy, the mother loses
approximately 800 milligrams of iron. Thus, women typically manifest hemochromatosis
later, most commonly after menopause.
The liver is
usually the first organ affected, and hepatomegaly is the most common initial
physical finding. Untreated, it can progress to cirrhosis, accompanied by portal
hypertension and varices. Hepatocellular carcinoma occurs in approximately 30% of
those who develop cirrhosis and is the most common cause of death in patients being
treated for hemochromatosis.
Other common
complications include cardiac dysrhythmias and congestive heart failure; diabetes
mellitus from pancreatic involvement; hypogonadism and various hormonal
deficiencies from testicular, pituitary and adrenal dysfunction; and arthritis
– with the involvement of the second and third metacarpophalangeal joints
(MCPs) a classic early finding. Excess iron also leads to increased
susceptibility to infection from siderophilic bacteria, most commonly, Vibrio
vulnificus, Listeria monocytogenes, and Yersinia enterocolitica.
Because many
complications of hemochromatosis are not reversible, early diagnosis and
treatment are critical for prevention. Features commonly reversed by treatment include
fatigue, depression, abdominal discomfort, and bronze discoloration of the skin.
Screening assays
for estimating total body iron stores are the serum iron level with percent transferrin
saturation (serum iron divided by total iron-binding capacity), and the serum
ferritin concentration. Every one microgram per liter increase in the serum
ferritin concentration represents an increase of approximately five milligrams of
iron stores.
Elevated ferritin
alone is nonspecific, requiring a detailed history and physical with repeated lab
studies to rule out other causes. With that in mind, if either the percent
transferrin saturation or the serum ferritin concentration is elevated, genetic
testing is recommended.
For those with
results consistent with hemochromatosis, evaluation of the liver is critical to
assess for the presence of cirrhosis. Over the past few years, improvements in lab
studies, ultrasound, and magnetic resonance imaging (MRI) have significantly
decreased the need for liver biopsy. For example, if the transaminase levels are
normal, the serum ferritin is below approximately 1000 micrograms per liter,
there is no hepatomegaly, and the patient does not drink excess alcohol, the
risk of cirrhosis is extremely low. Also, MRI with T2* calculation is an accurate
method for estimating hepatic iron content and has the advantage of being able
to assess cardiac iron deposition. When there is a borderline case, or whenever
there is doubt, liver biopsy remains the gold standard for diagnosing cirrhosis.
Treatment of
hemochromatosis involves removing the excess iron – via bleeding. Phlebotomy
presents a very simple treatment in an age of increasing medical complexity, which
is often a great relief to patients. This involves removing one pint (approximately
500 milliliters) of blood per session, which, depending on the patient’s
hematocrit, contains between 200 to 250 grams of iron. Aside from treating the
hemochromatosis patient, an advantage of phlebotomy is that the blood can be
added to the donor pool (after standard blood screening).
Initially, phlebotomy
is performed one to two times per week, as tolerated by the patient. It is then
tapered to monthly, and then eventually to every few months, in order to maintain
a ferritin level around 50 micrograms per liter or less. Since the average
hemochromatosis patient has excess stores of about ten grams of iron, this represents
approximately fifty phlebotomy sessions (not counting on-going iron absorption).꙳
For those with hemochromatosis, all adult
first-degree relatives require genetic counseling and lab studies. In the case
of children, testing the other parent usually suffices to determine their risk.
If this is untenable, the child can wait until eighteen years of age to undergo
genetic testing, given the time course of the disease.
For those who are asymptomatic and have
no family history, the United States Preventative Health Task Force has come to
no conclusions regarding screening. Arguments against screening involve the
high costs of testing for a disease with variable penetrance (not everyone with
the gene defect develops iron overload) and potential discrimination against
patients by the insurance industry.
Given the high prevalence in those of
northern European ancestry and the significant morbidity and mortality associated
with untreated hemochromatosis, more experts are recommending at least targeted
screening of late. They also recommend screening with genetic testing in order to
detect those who have not yet developed iron overload, especially as these costs
continue to decrease. Aside from these benefits, negative screening results are
also helpful in relieving significant anxiety for patients and their families.
꙳ 1 ml RBCs = 1mg iron; a patient with a 40% hematocrit
undergoing 500 ml phlebotomy loses 200 mg iron
References
Hemochromatosis, (2014), Retrieved from niddk.nih.gov/health-information/liver-disease/hemochromatosis (Accessed 03 October 2019).
Jameson, J.L., Fauci, A.S., et al,
(Eds.)(2018). Harrison’s principles of internal medicine. 20th edition.
New York: McGraw-Hill Education.
Kelley M, Joshi N, Xie Y, Borgaonker
M. Iron overload is rare in patients homozygous for the H63D mutation. Can J
Gastroenterol Hepatol. 2014;28(4):198-202.
Screening for hemochromatosis: recommendations
from the U.S. preventive services task force. Ann Intern Med. 2006;145:I-18.
doi: 10.7326/0003-4819-145-3-200608010-00002
Whitlock EP, Garlitz BA, Harris EL, et al.
Screening for hereditary hemochromatosis: a systematic review for the U.S.
preventive services task force. Ann Intern Med. 2006;145:209-23. doi:
10.7326/0003-4819-145-3-200608010-00009