In August 2019, the U.S. Food and Drug Administration (FDA) approved a new antibiotic for community-acquired bacterial pneumonia (CAP) and acute bacterial skin infections. Lefamulin (Xenleta, Nabriva Therapeutics) is in a class of antibiotics known as the pleuromutilins and represents the first antibiotic developed for systemic use in humans with a novel mechanism of action in over a decade (retapamulin was approved in 2007 for topical use).

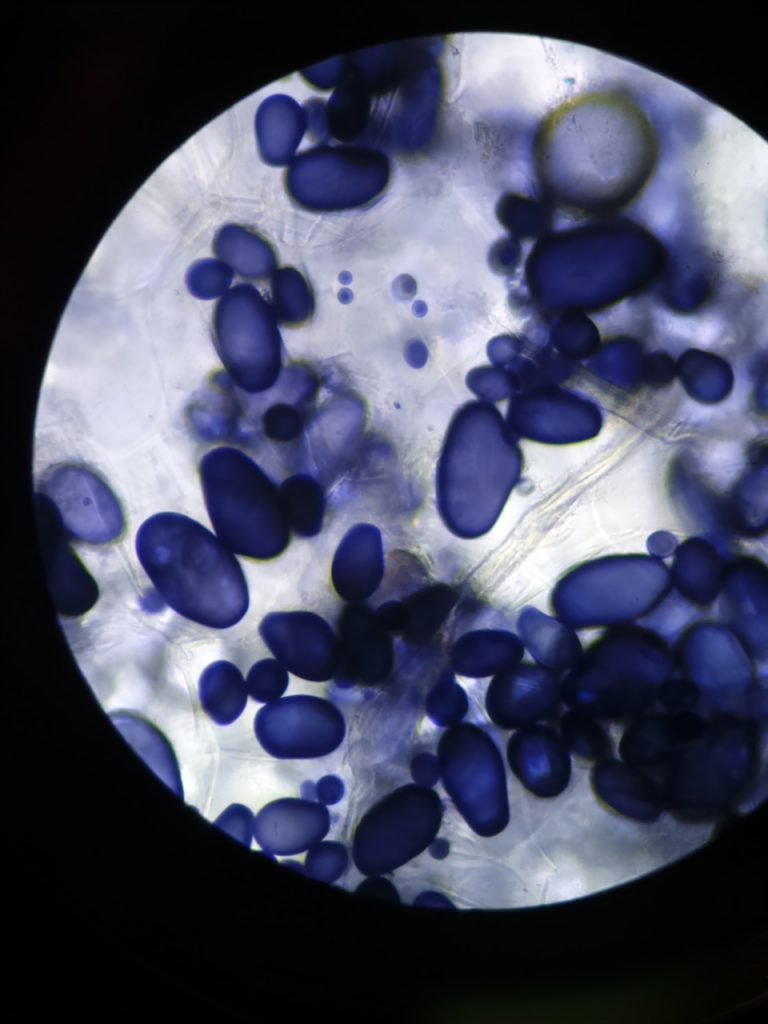
Pleuromutilins were discovered in 1950 from the fungi Pleurotus mutilis and Pleurotus (now Clitopilus) passeckerianus (the pleuromutilins were not named for the membranes surrounding the lungs).
Like clindamycin, linezolid, and the macrolides, the pleuromutilins block bacterial protein synthesis via binding to the 50S ribosomal subunit. They bind at a different site on the subunit such that there is no cross-resistance with other antibiotics.
Lefamulin shows robust activity against gram-positive and fastidious gram-negative bacteria, and the organisms often referred to as “atypicals,” such as Mycoplasma pneumoniae, Chlamydophila pneumoniae, and Legionella pneumophila.
Lefamulin has equivalent oral and intravenous bioavailability and can be taken with or without food, making the oral formulation a convenient option. It also has a good safety profile, the most common side effects being diarrhea and nausea. More rarely, hepatic enzyme elevation has been observed, and concomitant administration with cytochrome P450 (CYP) 3A4 inhibitors should be avoided due to the risk of QT-prolongation.
Given the trend toward worsening bacterial resistance against current CAP antibiotics and the increasing number of FDA warnings concerning quinolones, lefamulin looks to be a promising addition to the antibiotic armamentarium. Antibiotic stewardship programs should be reinforced to maintain its excellent efficacy and resistance profiles.